800-487-3808
800-487-3808

While it’s normal for those with dementia to feel worn out at the end of the day, some people can experience extreme changes in moods, cognition, and behavior once the sun begins to set.
If you, or someone you know, becomes aggressive, confused, sad, or anxious each evening, you may be dealing with a case of sundowner’s syndrome.
Sundowner’s syndrome, or "sundowning," isn’t a syndrome or a disease but rather a set of symptoms which typically occur in older adults in the late afternoon and evening.
It mainly affects people with Alzheimer's disease and other forms of dementia—with up to 20 percent of people with Alzheimer’s experiencing sundowner’s.
However, it is also experienced by people with other medical issues or those who spend time in a hospital or care home but have not been diagnosed with dementia.
Sundowner's is associated with a wide variety of symptoms and behaviors including:
The symptoms and their severity vary from person to person. One of the only consistent factors is the time of onset: as the sun starts to set, and darkness falls. Symptoms may get worse as the night progresses, and usually disappear within one hour of sunrise.
Some evidence suggests that sundowner’s symptoms are worse during winter when periods of sunlight are reduced.
Experts are still unsure as to why this phenomenon occurs, although there are some generally accepted theories.
 Those with dementia are at an increased risk for developing sundowner's syndrome. ( Image Reference )
Those with dementia are at an increased risk for developing sundowner's syndrome. ( Image Reference )
According to the Alzheimer’s Foundation of America, sundowner’s Syndrome may be caused by damage to the body’s internal clock, which happens in those with dementia. This affects sleep-wake cycles. The Foundation also advises that people with dementia struggle to process information which can cause fatigue, exhaustion, and irritability toward the end of the day.
Other factors which may contribute to symptoms of sundowner’s include:
While sundowner’s syndrome is typically associated with dementia, the symptoms can also be seen in people without dementia thanks to hospital settings, strong medications, severe pain, medical procedures, infections, and certain bodily processes.
Hospitals are notorious for causing sleep deprivation, thanks to the constant hustle and bustle. Patients are frequently awoken by other patients, beeping machines, bright lights, and by doctors and nurses who wish to take blood samples, check vital signs, and administer medications.
Boredom and lack of mobility mean that daytime naps are frequent and drawn out. Medications cause a false sense of exhaustion. Illness and pain lead to patients sleeping more.
In addition, the anxiety of being in a strange setting and out of routine, and the worry caused by illness and injury, further compound sleep problems.
All of these factors affect a person’s natural sense of tiredness, of night and day, of darkness and light. As a result, their biological clock becomes affected, their sleep-wake cycle is thrown off, and confusion and agitation ensue.
Even if you recover at home, recovering post surgery can manifest the same effects.
People who already have vision problems may experience difficulties once night falls. They tend to be even more sensitive to dwindling levels of light and may see twilight shadows as more confusing and menacing than most.
Low blood pressure, which may occur in older adults after eating, temporarily takes oxygen away from the brain and causes dizziness, confusion, and blurred vision. Low blood pressure can also be caused by surgery, or as a side-effect of certain medications.
Low blood sugar (hypoglycemia) leads to agitation and confusion. Hypoglycemia is caused by:
People with diabetes can experience hypoglycemia due to issues with blood sugar control.
Some doctors theorize that these factors—along with other conditions and bodily processes that can affect hearing, sight, and cognition—may contribute to sundowner's in those with and without dementia.
Many people, particularly older adults or those in hospital settings, are given high doses of medications which may contribute to the onset of confusion and delirium.
While sundowner’s syndrome may never completely disappear in those susceptible to it, there are certain steps that can be taken to manage symptoms and lessen their severity.
Options include lifestyle changes and medications.
There are several methods to manage the symptoms of sundowner’s, for yourself or for a loved one.
Different things trigger sundowner’s symptoms in different people. For one person, it could be changing light levels, for another, it could be low blood sugar at bedtime.
To help identify triggers, keep a note of daily activities, behaviors, meals, and surroundings. Look for patterns which may be contributing to symptoms.
Once these triggers have been identified, the situations that exacerbate symptoms can be avoided.
 Going to sleep at the same time each night will lessen the effects of sundowner's syndrome. ( Image Reference )
Going to sleep at the same time each night will lessen the effects of sundowner's syndrome. ( Image Reference )
A daily routine—with regular waking and bed times—will help create stability and reduce stress and confusion in those affected. It may be helpful to schedule appointments, excursions, shower times, and other events for earlier in the day, before fatigue sets in, and the sun begins to go down.
If it’s necessary to adjust the routine, it’s best to do so over time, to lessen the impact of change.
Mealtimes should also follow a schedule.
Large meals, particularly before bed, may interfere with blood sugar regulation, and therefore increase confusion, dizziness, and irritability.
On the other hand, low blood sugar from missed or irregular mealtimes can also contribute to symptoms. Three meals a day, with light snacks as needed, will help with blood sugar regulation and contribute to a good night’s sleep.
Avoid rich foods, fatty or fried foods, spicy dishes, citrus fruits, and carbonated drinks before bedtime. These can cause indigestion or heartburn, which disrupt sleep.
It’s worth consulting a dietician or nutritional therapist if you are unsure of the best foods and mealtimes to manage sundowner’s symptoms.
In addition to managing mealtimes, it’s important to also limit or avoid foods, drinks, and other items which stimulate the mind as these can interfere with sleep, cause blood sugar fluctuations, and contribute to confusion and fatigue.
Common stimulants include:
Watching television at night or vigorous activity close to bedtime are also considered stimulative.
The National Sleep Foundation defines sleep hygiene as “a variety of different practices and habits that are necessary to have good nighttime sleep quality and full daytime alertness”.
Important sleep hygiene practices—which should be tailored to each individual based on their needs and preferences—include:
This can improve mood and alertness. Naps should not occur within four hours of bedtime.
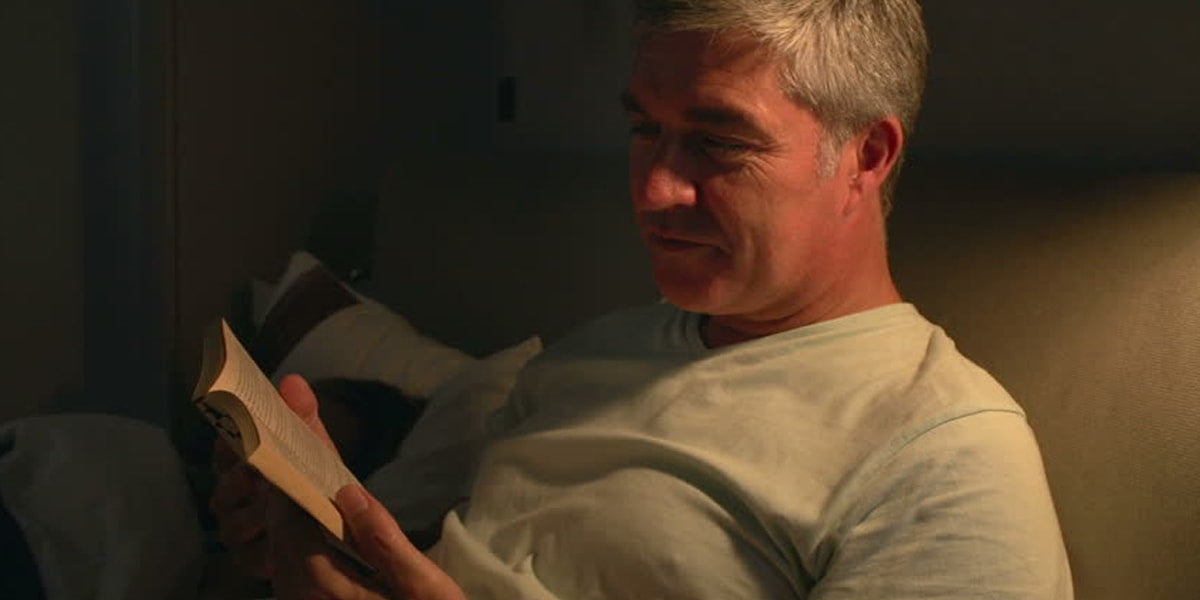 Not only is a good book before bed pleasant, it actually alleviates the symptoms of sundowner's syndrome. ( Image Reference )
Not only is a good book before bed pleasant, it actually alleviates the symptoms of sundowner's syndrome. ( Image Reference )
This trains the body to know when it is time for sleep and can help avoid the confusion and agitation experienced by those with sundowner's. A relaxing routine could include a bath, reading a book, listening to soothing music, diffusing lavender essential oil, or engaging in some light stretching.
Comfortable mattresses, pillows, and nightwear are important. A room temperature of between 60 and 67 degrees is optimal for a good night’s sleep. Subdued lighting, blackout curtains, ‘white noise’ machines, humidifiers, and fans can all aid sleep quality.
 Treat your body right, with regular exercise, to feel better and sleep better. ( Image Reference )
Treat your body right, with regular exercise, to feel better and sleep better. ( Image Reference )
Regular physical activity is vital for a healthy mind and body, at every age! Those with sundowner’s and dementia will benefit from daily movement as staying sedentary all day can interfere with quality sleep.
Exercises should be tailored to the individual and can include anything from a gentle stroll to gardening, swimming, dancing, or using a stationary bicycle. Yoga is a fantastic option for seniors because of its low-impact movements. Click here to learn more about yoga for seniors.
It’s best not to exercise within four hours of bedtime as this can disrupt sleep.
 Fight sundowner's syndrome with sunshine. Natural light will improve your mood and your health. ( Image Reference )
Fight sundowner's syndrome with sunshine. Natural light will improve your mood and your health. ( Image Reference )
Well-lit rooms can boost the mood and energy levels, and a whole host of research extols the benefits of natural light for regulating our hormones and natural internal clocks.
Those with sundowner’s disease should enjoy some natural light each day—by taking a daytime stroll or sitting by a large window. If it’s not possible to enjoy the natural rays, daily use of a special light therapy box or a full-spectrum fluorescent light can be beneficial.
A review of research, published in 2011, recommends light therapy to reduce agitation and confusion in people with dementia.
As evening approaches, bright rooms can distract from falling levels of outside light. The Alzheimer’s Association recommends brightening indoor lights if confusion or agitation is experienced.
Stress leads to increased confusion and agitation in those prone to sundowner’s syndrome.
As part of the wind-down before bed, it’s a good idea to keep the evenings as quiet and relaxing as possible.
Close the curtains and turn on the lights, and maintain a pleasant temperature in the room. Ensure noise levels, from family members and television sets, are kept to a minimum.
Relaxing music, foot massages, and calming scents like lavender can all help soothe and pacify. Pets can be especially relaxing—with results revealing that animals help reduce feelings of anxiety and sadness in people with dementia.
If someone with sundowner’s disease needs to stay in the hospital, it may be helpful to provide items that create feelings of comfort and familiarity in an otherwise strange and unpredictable setting.
Family photos, favorite blankets, familiar foods, and other valued items can all help lessen the fear and confusion surrounding a hospital stay.
Doctors and nurses should be informed if a patient is prone to sundowner’s syndrome.
If the above tips don’t reduce symptoms as much as desired, then medication is another option.
The following medical treatments are available, and are best used in conjunction with the lifestyle changes listed above:
Research indicates that a low dose of melatonin may ease symptoms of sundowners. Melatonin is a hormone that occurs naturally in the body and plays a role in regulating the body’s natural sleep-wake cycle.
Some antidepressants have been shown to reduce agitation, aggression, and anxiety in those with dementia.
However, these medications may have other side effects so it’s important to discuss all options with a doctor.
Seeing loved ones act in strange and unpredictable ways can be extremely upsetting and frightening for family members. If you are looking after someone with sundowner’s, it’s important to take care of your own physical and mental health too.
 Caregivers should never neglect their own health. Stay fit and active, and don't forget to spend time with your loved ones. ( Image Reference )
Caregivers should never neglect their own health. Stay fit and active, and don't forget to spend time with your loved ones. ( Image Reference )
Make sure to:
While the above tips are useful for both those with sundowner’s and those caring for people with the condition, there are some additional tips that can be helpful for carers as sunset approaches:
 Sundowner's syndrome is not the end of the world. There are ways to manage the symptoms and live your best life! ( Image Reference )
Sundowner's syndrome is not the end of the world. There are ways to manage the symptoms and live your best life! ( Image Reference )
While sundowner’s syndrome can seem like a scary and worrying condition, there are many options available to those who experience negative symptoms as the day draws to a close.
Treatment for sundowner’s syndrome is not a one-size-fits-all plan—what works for one person may not work for another. That’s why it’s important to continue to explore many different avenues. Don't be afraid to accept help, stay positive, and lean on support systems … because the sun always rises!
Finally, remember to discuss any type of new or strange behavior with a doctor. Don’t automatically assume that agitation or confusion in the evening is sundowner’s, or even dementia-related. Restlessness, agitation, sleep issues, and other behaviors may be symptoms of mental health issues such as depression or anxiety, or physical ailments like infection or hypoglycemia.
Sources:
http://www.alzfdn.org/EducationandCare/sundowning.html
http://www.alz.org/care/alzheimers-dementia-sleep-issues-sundowning.asp
Comments
Leave a comment